Transcatheter Aortic Valve Implantation (TAVI) – The Most Advanced severe aortic stenosis therapy – A boon for patients who can not undergo Open Heart Surgery
Robot Assisted Heart Procedures are done to treat a variety of conditions
Get Free Expert Medical Advice/ Second Opinion from Top Heart Specialists in India by Email, WhatsApp or Viber.
If you are an adult in need of an aortic valve replacement and not well enough to have heart valve surgery, you will benefit from TAVI procedure that helps to improve a damaged aortic valve.
Transcatheter aortic valve implantation (TAVI) has become the an acceptable option for elderly high-risk patients presenting severe and symptomatic aortic valve stenosis. Request a Call Back
Request a Call Back
Why you should choose India for Affordable, World Class Heart Surgery, Cardiac Care ?




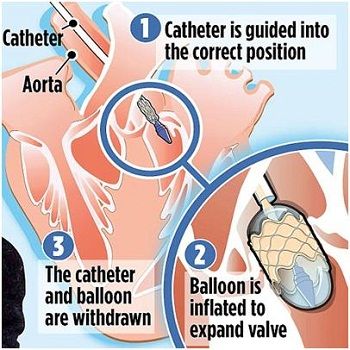
TAVI (Transcatheter Aortic Valve Implantation)
Aortic stenosis, the narrowing of the aortic valve, which affects the supply of blood from the heart to the rest of the body, is one of the most frequently acquired heart valve diseases.
Till 2002, replacement of the aortic valve through an open heart surgery, putting the patient on “heart-lung machine”, was the standard mode of treatment.
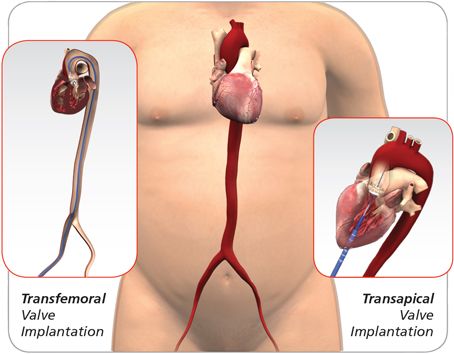
For a significant number of high-risk, in-operable elderly, a new minimally invasive procedure, transcatheter aortic valve implantation (TAVI), has emerged as a safe and viable option.
TAVI does not require the patient to be on the heart-lung machine. The new bioprosthetic valve is implanted using a catheter, inside the calcified valve itself, through the femoral vein (transfemoral) or the transapical approach.
TAVI, pioneered in 2002, has significantly changed the field of aortic valve replacement. Till date, some 70,000 procedures have been done in some 500 centres the world over, dramatically changing the manner in which the high-risk elderly are treated. TAVI procedure is currently being performed on only those patients who are not suitable for open-heart surgery.
The aortic valve regulates the flow of oxygen-rich blood from the heart into the main blood vessel leading to the rest of the body. It is composed of three triangular-shaped flaps that fit neatly together.
As the main chamber of the heart contracts, the flaps open up and allow blood to enter into the artery. They then slap shut to prevent blood from flowing back into the heart. As with other parts of the body, over a long period of time this valve can wear out and become dysfunctional.
Aortic-stenosis is, for the most part, a chronic degenerative process of aging. About 7 per cent of people over the age of 65 develop aortic stenosis.Get Estimate
Advantages of Transcatheter Valve Implantation (TAVI)
Benefits of TAVI include a shorter procedure, less pain, and a shorter stay in the hospital. Because it is non-invasive, recovery time is significantly shorter than after open-heart surgery – about 2 to 4 weeks instead of 6 to 8 weeks. As with surgical heart valve replacement, TAVI provides both short- and long-term relief of symptoms, normal aortic valve function and improvement in your overall life expectancy and functioning.Get Estimate
LVAD/ VAD Left ventricular Assist Device or Ventricular Assist Device
Left ventricular Assist Device or Ventricular Assist Device was once considered as a stop gap arrangement or a bridge to transplant in patients for end stage heart failure who were waiting for heart transplant. With advancement in medical technology, the quality of LVAD has improved to such an extent that patients have shown improvement in quality of life to a great extent
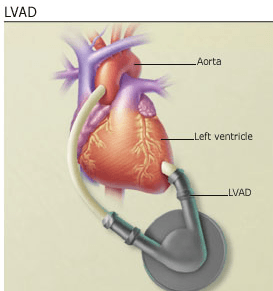
A tube passes from the device through the skin. This tube, called the driveline, connects the pump to the external controller and power source.
The pump and its connections are implanted during open-heart surgery. A computer controller, a power pack, and a reserve power pack remain outside the body. Some models let a person wear these external units on a belt or harness outside.
The power pack has to be recharged at night.
Benefit of LVAD involves restoration of blood supply to the heart and other vital organs, time to rest for the heart, reduced fatigue and discomfort.
Side effects include infection, internal bleeding, heart failure, kidney failure, stroke, device failure, blood clot and respiratory failure.
Implantable Cardiac Defibrillators
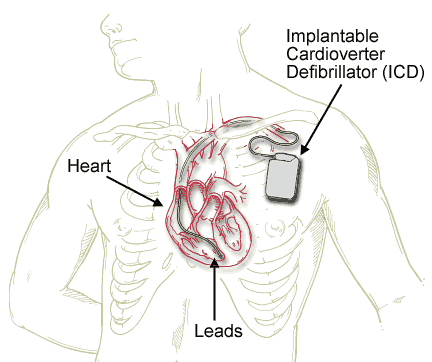
The device is made up of a battery operated pulse generator and a set of leads. The device is placed under the skin near the collar bone or waistline and the leads are connected to the heart. The device is implanted under general anaesthesia and does not require open heart surgery. Once fitted, the device is tested before the patient is allowed to go home. The device records normal rhythm, recognizes abnormal rhythm, delivers shocks and records the date and time of event.
Cardiac Resynchronisation Therapy- CRT
The battery operated device sends small, undetectable electrical impulses to both lower chambers of the heart to help them beat in a more synchronized pattern. The leads between the heart and the device carry electrical signals to and fro. This improves the heart’s ability to pump blood and oxygen to the body.
Implantable device system has a programmer, an external computer located in your doctor’s office or clinic that is used to program the heart device and retrieve information from your heart device that will assist your doctor in your heart failure treatment.
CRT pacemaker and a combination CRT pacemaker with defibrillation therapy help to coordinate the heart’s pumping action and improve blood flow. They can also speed up a heart that is beating too slowly.
In addition the CRT pacemaker with defibrillation therapy (CRT-D) also offers the ability to detect and treat dangerously fast heart rhythms, which some individuals with a damaged heart muscle may be at risk for developing.Get Estimate

 Click to WhatsApp
Click to WhatsApp +91-9899993637
+91-9899993637






 Get Expert Medical Opinion/ Second Opinion – Send us the Medical reports by Email or WhatsApp and we will get you Expert Advice and Treatment Cost Estimates from Top Specialist at Three of India’s leading hospitals within 48 hours.
Get Expert Medical Opinion/ Second Opinion – Send us the Medical reports by Email or WhatsApp and we will get you Expert Advice and Treatment Cost Estimates from Top Specialist at Three of India’s leading hospitals within 48 hours. Free Concierge Services – Once you decide to come to India, We will arrange Priority Scheduling of Hospital Appointments, Travel & Visa Assistance, Airport Pick up, Economical Hotel Stay, Complete Local Support 24X7.
Free Concierge Services – Once you decide to come to India, We will arrange Priority Scheduling of Hospital Appointments, Travel & Visa Assistance, Airport Pick up, Economical Hotel Stay, Complete Local Support 24X7.


