
Polyps may be small and produce few, if any, symptoms. For this reason, doctors recommend regular screening tests to help prevent colon cancer by identifying polyps before they become colon cancer.
Cancer is ultimately the result of cells that uncontrollably grow and do not die. Normal cells in the body follow an orderly path of growth, division, and death. Programmed cell death is called apoptosis, and when this process breaks down, cancer results. Colon cancer cells do not experience programmatic death, but instead continue to grow and divide. Although scientists do not know exactly what causes these cells to behave this way, they have identified several potential risk factors.
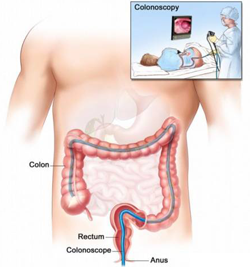
How is colon cancer diagnosed and staged?

A colonoscopy is a procedure where a long, flexible tube with a camera on one end is inserted into the rectum to inspect the inside of the colon. If polyps are found in the colon, they are removed and sent to a pathologist for biopsy – an examination under a microscope that is used to detect cancerous or precancerous cells. A barium enema begins with the patient swallowing a special liquid that contains the element barium. After the barium lines the large intestine, an x-ray of the colon and rectum is taken. Tumors and polyps will appear as dark shadows on the x-ray. If a colon cancer diagnosis is made after a biopsy, doctors will often order chest x-rays, ultrasounds, or CT scans of the lungs, liver, and abdomens to see how far the cancer has spread. It is also not uncommon for a doctor to test blood for CEA (carcinoembyonic antigen) – a substance produced by some cancer cells.
Minimal Invasive Laparoscopic Colon Cancer Surgery
- The surgeon enters the abdomen by placing a canula (a narrow tube like instrument) into the abdomen (belly) through a small incision (½ — ¼ inch)
- Carbon Dioxide gas is pumped into the abdomen through the port (cannula) to puff-up or inflate the belly, making working room for the surgeon.
- A laparoscope (a tiny telescope connected to a video camera) is placed through the canula, and allows the surgeon to see a magnified lighted view of the internal organs on a TV monitor
- 2 to 4 other canulas are inserted to allow use of special instruments to work inside the abdominal cavity (belly).
- If a portion of the colon is removed, one of the small canula incisions is slightly enlarged to permit removal of the tissue.
Advantages of Minimal Invasive Laparoscopic Colon Cancer Surgery
- Minimally invasive, Less surgical trauma, shorter hospitalization, Improved cosmetic results
- Reduced post operative pain, faster recovery and return to daily activities and normal diet.
- Less postoperative pain killer requirement
To know more about “Colon Cancer Treatment” in India please this links https://safemedtrip.com/medical-services/cancer-treatment-in-india/colon-cancer-treatment-in-india.html

 Click to WhatsApp
Click to WhatsApp +91-9899993637
+91-9899993637



