Thyroid cancer is fairly uncommon, accounting for only 1.2% of all new cancers . Although 
Thyroid malignancy is the most common endocrine malignancy. Thyroid cancer accounts for more than 90 per cent of all endocrine malignancies, but represents only about one per cent of all human cancers. The worldwide incidence of thyroid cancer is approximately 1,40,000. The excellent long term survival rates seen in patient who have thyroid cancer is reflected in the relatively small number of disease-specific deaths attributable to thyroid cancer compared with other malignancies.
Recently, in some regions of the world the incidence of thyroid cancer has been increasing. However, evidence supports that the increase in incidence appears to be due to improved detection rather than an increase in the true occurrence, and may reflect differences in access to healthcare. Unlike most head and neck tumours, thyroid cancer is more common in women and often follows a protracted natural history.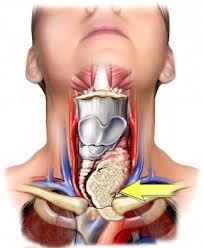
Types of thyroid cancers
Thyroid cancers encompass varied histologies ranging from indolent to aggressive. They may be classified into:
- Differentiated carcinomas, such as papillary carcinoma, follicular carcinoma and Hurthle cell carcinoma account for 90 per cent of the thyroid cancers diagnosed.
- Medullary cancer arising from the parafollicular cells account for three per cent.
- Anaplastic (undifferentiated) carcinoma.
Symptoms

- Rapid growth
- Suspicious criteria by ultrasonographic examination
- Vocal cord paralysis
- Family history of thyroid cancer
- Prior history of radiation exposure during childhood
- Hard fixed nodule
- Palpable cervical lymphadenopathy
Evaluation
- Fine-needle aspiration (FNAC) has the highest sensitivity and specificity for identification of malignant thyroid nodules. Thyroid function tests are almost uniformly normal. Even though FNAC is highly sensitive and specific, follicular thyroid cancers can’t be diagnosed by FNAC.
- A surgical biopsy or a hemithyroid specimen is required for a confirmatory diagnosis.
- Ultrasound evaluation or CT scan imaging is required to document the extent of the primary disease and to exclude any nodal involvement in the neck.
Treatment
- Thyroidectomy: For differentiated thyroid cancer of more than one cm, total (near total) thyroidectomy is the preferred operation.
- Lymph node dissection is carried out only for patients who have known lymph node metastases detected on preoperative staging or intraoperatively.
- Role of radioactive iodine: Radioactive iodine (RAI) ablation is carried out one to four weeks after surgery in most papillary thyroid cancers greater than one cm.
- Role of external beam irradiation in initial therapy: External Beam Radiation Therapy (EBRT) is most often used for unresectable tumours that do not concentrate RAI, or for older patients above 45 years who have evidence of gross extrathyroidal extension of the tumour into surrounding structures that are likely to have microscopic or small volume macroscopic disease that is not amenable to RAI therapy.
- Role of chemotherapy is usually palliative in the treatment of thyroid cancers.
- Monitoring for recurrent/persistent disease is carried out with six-monthly thyroglobulin (Tg) estimation and ultrasonography
- Medullary thyroid cancers are an aggressive variety with high propensity for nodal involvement, and hence the treatment involves total thyroidectomy with lymph node dissection.
- External beam radiotherapy is advocated for treating surgically unresectable residual or recurrent disease.
- Adjuvant irradiation is recommended for extrathyroidal disease, extensive nodal involvement, or extracapsular spread.
- Post treatment monitoring for recurrent disease is done with serum calciton in estimation.
- Treatment results for anaplastic carcinoma are discouraging. Despite the employment of various aggressive treatment strategies that consist of surgery, radiation therapy, chemotherapy, or combinations of the three, almost all patients with this disease die a cancer related death. The median survival of anaplastic thyroid cancer is two to six months, and only a few patients have survived for more than 12 months. Hence the goal of treatment is usually palliative.
To know more about Thyroid Cancer in India please visit this link : https://safemedtrip.com/medical-services/laparoscopic-minimally-invasive-surgery-in-india/thyroidectomy-in-india.html

 Click to WhatsApp
Click to WhatsApp +91-9899993637
+91-9899993637



