
The condition affects, mostly those over age 50. The symptoms of spinal stenosis are numbness, weakness and cramping or pain in the legs, thighs or feet, which interferes with the ability to walk. While symptoms of spinal stenosis start slowly and tend to worsen over time, leg pain can become so severe that sufferers find themselves unable to stand or walk for more than a few minutes.
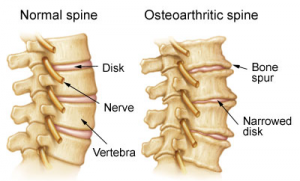
“Spinal stenosis doesn’t really cause back pain but pain that radiates down into buttocks and lower legs,” says neurosurgeon at a leading hospital in United States. “The narrowing of the spinal canal reduces blood flow to nerves in the lower back.” The pain often diminishes or disappears altogether when a patient is sitting or lying down – unlike a pinched nerve caused by a bulging disk, which may hurt all the time.
While a pinched nerve due to a protruding disk often resolves on its own, there’s no cure for spinal stenosis. Regular exercise can help maintain blood flow to the nerves to reduce leg pain and numbness. People can help keep their mild symptoms from turning severe by staying active. Many patients, however, are unable to exercise by the time they receive a diagnosis, and are often caught in a vicious cycle of forced inactivity, which only exacerbates symptoms.
The goal is to get patients up and walking again, but surgery won’t take away back pain caused by other factors like arthritis and patients need to understand that.”
If you have spinal stenosis and determine that surgery is best for you, here are options to consider:
Lumbar Laminectomy: This is the traditional approach, also called decompression surgery, where surgeons create space by removing the lamina, the part of the vertebra that covers spinal canal. Laminectomy enlarges the spinal canal to relieve pressure on the spinal cord or nerves, and has about an 80 percent success rate at improving walking abilities. In some cases, surgeons also perform spinal fusions, connecting two or more bones in the back, to help stabilize the spine.
The downside to the traditional open laminectomy is a longer recuperation time because surgeons need to disrupt more tissues and muscles to get to the lamina. Serious complications can occur in rare cases including blood clots in the legs and spinal cord injury that results in weakness or numbness.
Minimally Invasive Laminectomy: It involves tiny incisions through which a small camera, called a laparascope, and surgical tools are inserted to perform the lamina removal and spinal fusion if needed – and has a much faster recuperation time.
Patients often find it easier to walk immediately after the procedure is performed, and often experience only a few days of soreness as the incisions heal, rather than the few weeks of healing associated with a traditional laminectomy. Complication rates are similar for both types of this procedure.
For more information on Minimally Invasive Spine Surgery, Please visit this link: https://safemedtrip.com/medical-services/spine-surgery-treatment-in-india/minimally-invasive-spine-surgery-in-india.html

 Click to WhatsApp
Click to WhatsApp +91-9899993637
+91-9899993637



