IVF Male and Female Infertility Treatment from Leading Hospitals in India
Excellent Outcomes and Affordable Cost is assured.
Comprehensive Treatments Options available in India to treat Infertility
Why you should choose World Class Hospitals in India for IVF, Male and Female Infertility Treatments?




At India’s leading IVF Clinics we have a scientific approach to diagnose the cause for infertility. Our IVF center has state-of-the-art facilities for (IVF), In Vitro Fertilization and fully functional laboratory for diagnostic and therapeutic tests. The world class facilities along with competent staff have enabled us to achieve an outstanding success rate. We provide everything under one roof and make best possible efforts to help infertile couples achieve their dreams of parenthood.
If the problem can be rectified our doctors will treat the problem and if the problem cannot be rectified then alternatives like IVF or Surrogacy are offered to the patient. During the entire treatment process the team of doctors at IVF India makes sure that the couple is comfortable, hopeful, emotionally strong and have clear understanding of the entire process.
Hundreds of International Patients who travelled long distance to India have benefitted from the expertise of renowned Indian doctors.
Comprehensive Treatments Options available in India to treat Infertility
IVF India has complete range of services to handle any kind of infertility with the best of professionals to back the best in class technology at work.
- In Vitro Fertilization (IVF).
- Intra Uterine Insemination(IUI).
- Intra Cytoplasmic Sperm Injection (ICSI).
- Blastocyst Culture.
- Sperm Aspiration) PESA (Percutaneous Epididymal Sperm Aspiration).
- Advanced Treatment Options like TESE (Testicular Sperm Extraction) MESA (Microsurgical Epididymal ).
- Cryopreservation.
- Laser Assisted Hatching.
- Embryo Transfer.
- Ovulation Induction.
- Egg Donation/Egg Sharing.
- Zona free Embryo Transfer.
- Semen Bank
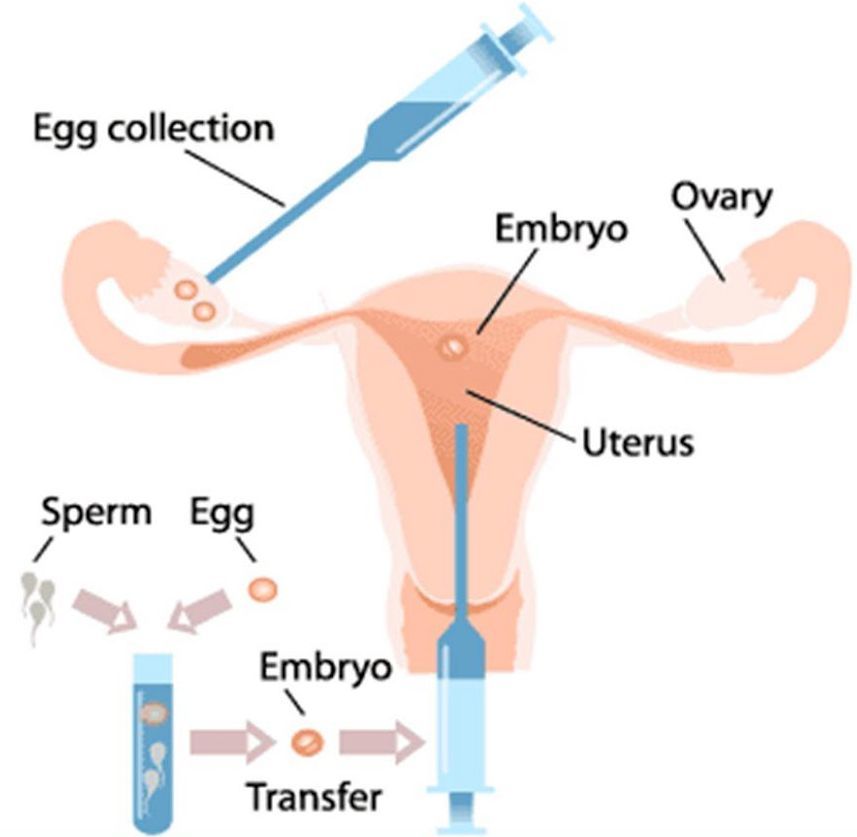
IVF (In Vitro Fertilization)
IVF means fertilization of egg and sperm outside the body in a test tube. Since the birth of Louise Brown, the first test-tube baby in 1978, IVF has resulted in more than 120, 000 babies worldwide. Pregnancy rates and live birth rates have improved over the past few years, leading to a steady increase in the number of IVF treatment cycles performed worldwide.
An understanding of natural conception is important in order to understand in-vitro-fertilization or IVF as commonly known. Normally, a woman will produce a mature egg each month. The egg (oocyte) is released from the ovary at the time of ovulation and transported to the fallopian tube.
Usually, it is in the fallopian tube that it will encounter sperm and be fertilized. The fertilized egg develops into an embryo that will travel to the womb where it attaches and grows.
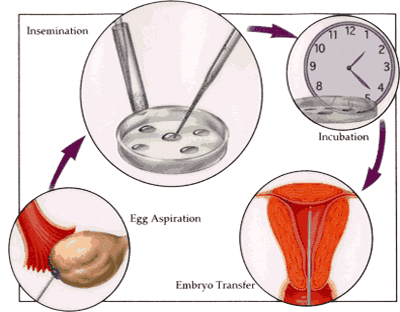
Process followed during IVF Treatment Cycle
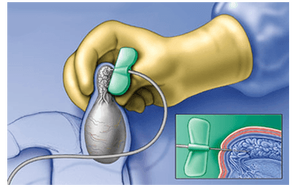
An IVF cycle consists of ovarian stimulation, egg collection, fertilization, embryo culture and embryo transfer. Ovarian stimulation consists of daily injection of hormones to the female partner with frequent clinical and ultrasonographic monitoring. This usually continues for 10-15 days. Egg retrieval is performed under anaesthesia through the internal route. There are no incisions or scars.
The egg and sperm are either mixed (IVF) or the sperm is injected into the egg (ICSI-intracytoplasmic sperm injection).
The fertilized egg forms the embryo. The embryo is cultured in the laboratory for 2-3 days . Two-three best embryos are selected and transferred into the womb (uterus) on the second or the third day. The pregnancy test is done 14 days after the day of embryo transfer.Get Estimate
IVF Treatment is most useful for
-
Women with blocked, damaged Fallopian tubes.
-
Women with endometriosis.
-
Women with cervical mucus problems.
-
Men with infertility problems.
-
Men or women with immunological infertility problems.
-
Couples with unexplained infertility
IUI – Intra Uterine Insemination
Male Infertility Treatments
1. Intracytoplasmic Sperm Injection (ICSI)
ICSI has revolutionized the management of male infertility. Following egg retrieval, a single sperm is injected directly into an egg;. About 70 percent of eggs get fertilized. Fertilization is confirmed 18-24 hours after retrieval. ICSI is a highly successful technique used to help couples who have previously failed to achieve conception with standard IVF.
ICSI is highly beneficial for patients who are unable to conceive due to Low Sperm Count, Abnormally Shaped Sperm, Poor Sperm Movement. If a man does not have any sperm in his ejaculate, but he is producing sperm, they may be retrieved through testicular sperm extraction, or TESE. Sperm retrieved through TESE require the use of ICSI.
2. PESA (Percutaneous Epididymal Sperm Aspiration)
3. MESA (Microsurgical Epididymal Sperm Aspiration)
Microscopic Epididymal Sperm Aspiration (MESA) is a technique for the retrieval of sperm from the epididymis of men in whom transport of sperm from the testicle to the ejaculate is not possible because the drainage (ductal) system is absent or is not subject to reconstruction.
This problem most commonly occurs in men with vasal agenesis, a condition in which the vas deferens or drainage system of the testicle fails to develop prior to birth.
4. TESE (Testicular Sperm Extraction) Surgical Sperm Retrieval
Retrieval of sperm from the testis or epididymis is associated with good pregnancy rates using in vitro fertilization. Micromanipulation of gametes during assisted reproduction could improve these pregnancy rates.
Ms. Sherber from USA came to India for Successful IVF Infertility Treatments
It feels blessed to have a bundle of joy in our arms and Safemedtrip made our dream of becoming parents come true. It was a joyous experience here in India and I can honestly say that I can’t remember ever been taken care of by so many nice, kind, and caring people. I’m sure that many people will find it to be a big decision as I did to come to a different country not knowing anyone and worrying about the language barrier, and being so far from home.
But yet we came here with full support from the team of Safemedtrip who made sure that we met the experts in the field of infertility who guided us well throughout. For those who are apprehensive of coming to India for treatment, let me reassure you it is not a problem at all. They speak good English here and if there was ever a time when I had a small problem there was always someone there to help. As far as feeling homesick I felt that I had met many new friends.
We traded many stories between us. My husband came with me and we had spacious room and he had his own bed, TV, ice box, and a computer to our use to be able to keep in contact with our family.
Ms. Sherber, USA IVF, ICSI, IUI, Male & Female Infertility Treatments
Get the SafeMedTrip Advantage


No Obligation – Zero Cost Assistance. We do not collect any service fee from patients. You will directly pay the hospitals after you arrive in India. We ensure Quick, Hassle Free, Affordable Treatment at World Class hospitals in India.

 Click to WhatsApp
Click to WhatsApp +91-9899993637
+91-9899993637